Feeling a sharp pain when biting down or exposed to hot or cold foods? Does it linger even after the stimulus is gone? These are common signs of a cavity that has progressed deep into the tooth’s inner layers. But does a painful cavity always necessitate a root canal procedure?
While certain symptoms do warrant a root canal, others can be resolved with more conservative treatments. As with any complex health issue, it’s essential to understand the nuances in order to determine the appropriate course of action.
Let’s explore the causes of painful cavities, warning signs for root canals, interim pain relief, treatment alternatives, and preventive best practices.
I. If a cavity hurts does it mean a root canal?
No, a hurting cavity does not always mean a root canal is needed. The pain could be due to the cavity reaching the dentin or nearing the pulp, but the appropriate treatment depends on the extent of the decay and the condition of the tooth pulp.
1. What causes a cavity to hurt?
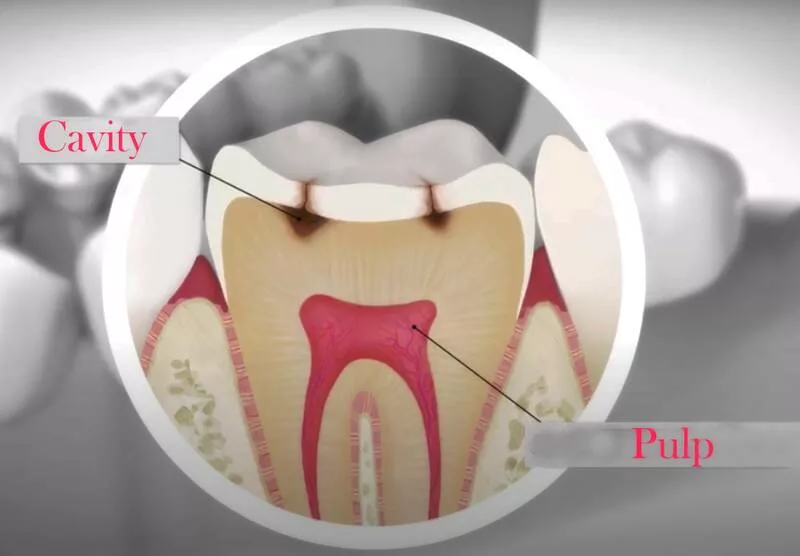
To understand why cavities become painful, it helps to first review tooth anatomy. Each tooth is composed of multiple layers, including the hard, outer enamel made of calcium phosphate, the softer dentin underneath containing nerve-rich tubules, and the innermost dental pulp containing nerves and blood vessels.
Tooth decay occurs when oral bacteria metabolize carbohydrates and produce acids that demineralize and erode the enamel. If the decay continues untreated, it penetrates the enamel to reach the more sensitive dentin.
This layer contains tiny tubules that connect to the tooth’s nerve center. Exposure to these tubules is often what causes pain and sensitivity, especially to temperature changes.
As the decay progresses deeper, it may eventually reach the pulp chamber at the center of the tooth containing nerves and blood vessels.
Bacteria can then infect this tissue, causing inflammation and irreversible damage known as irreversible pulpitis. This kind of infection is extremely painful and usually indicates a root canal is required.
So in summary, cavities become increasingly painful as they allow bacteria and external stimuli to reach the innervated layers of the tooth.
Enamel erosion causes no pain, but dentin exposure and pulp inflammation result in heightened sensitivity and often lingering discomfort.
2. Do painful cavities always need a root canal?
While it’s true that severe tooth pain can signal pulp infection requiring a root canal, not all painful cavities necessitate this intensive treatment.
The key factor is whether the bacteria and decay have reached and infected the pulp itself, not just the surrounding layers.
If a cavity is limited to the enamel and outer dentin but has not penetrated the pulp, a simple filling may suffice to replace the missing tooth structure and prevent further damage.
But once the pulp becomes irreversibly infected and inflamed, root canal therapy is generally required to remove the infected tissue and save the tooth.
Therefore, the extent of the decay and actual condition of the pulp will determine if a painful cavity warrants a root canal or another more conservative treatment.
To properly diagnose the cause of pain, dentists often take X-rays to visualize the internal tooth anatomy and test reaction to temperature stimuli.
In summary, severe, lingering pain does not automatically mean a root canal is imminent. While pain indicates decay has reached the inner layers, actual pulp infection and necrosis must be present before root canal therapy becomes necessary. Catching it early maximizes options.
3. Can I get a filling and not a root canal?
It is often possible to treat a painful cavity with a simple filling as long as the pulp remains free of infection. During the procedure, the dentist will numb the area, isolate the affected tooth, and then remove any decayed material.
The void is then filled with composite resin, amalgam, or another durable filling material.
As long as this restoration removes all the decay and seals the inner layers off from external stimuli, inflammation can resolve and sensitivity diminish without requiring a root canal.
However, if the pulp has already become infected due to extensive decay, a filling alone cannot save the tooth.
The filling itself should not cause discomfort. With anesthesia, the preparation process should be painless. Some temperature or pressure sensitivity is normal for a few weeks after the procedure as inflammation subsides and the tissue heals.
But infection-related pain requiring root canal therapy should not occur if the pulp remained relatively healthy.
Therefore, don’t assume your painful cavity necessarily warrants a root canal right away. Early intervention with a filling may allow you to avoid this intensive procedure.
Just be sure to see your dentist promptly at the first sign of pain or sensitivity.
4. Does tooth sensitivity to cold mean root canal?
Tooth sensitivity or pain when exposed to cold foods and beverages is one of the most common signs of tooth decay and possible pulp inflammation. But temperature sensitivity alone does not always indicate an inevitable root canal.
There are many potential causes for thermal sensitivity beyond just pulp infection, including:
- Exposed dentin from eroded enamel
- Gingival recession causes loss of protective enamel near the root
- Cracked or chipped teeth allow stimuli to reach the dentin
- Worn-down enamel from aggressive brushing
- Recent dental procedures like fillings, crowns, or whitening
- Chronic grinding or clenching habits
Additionally, external factors like dietary acidity and using cold products directly on teeth can heighten temperature sensitivity even in otherwise healthy teeth.
Therefore, while thermal sensitivity is something to discuss with your dentist, do not assume it directly translates to an inflamed or necrotic pulp.
Appropriate treatment depends on an examination of the tooth anatomy and direct pulp tests. Sensitivity could stem from various causes not requiring immediate root canal therapy.
II. What are the signs that you need a root canal?
Though pain level alone does not dictate the need for a root canal, certain symptoms in combination often do signal irreversible pulp infection and the need for urgent dental intervention. Signs it may be time to see an endodontist include:
# Severe Toothache
Constant, throbbing pain that keeps you awake at night or requires repeated pain medication indicates advanced tooth decay and possible pulp necrosis. Infection-induced inflammation pressurizes the rigid pulp chamber causing severe pain with chewing or temperature changes. Immediate evaluation is needed.
# Prolonged Sensitivity
Lingering hot/cold sensitivity or pain that remains even after the stimulus is gone suggests actual pulp inflammation rather than just exposed dentin. The pulp may be struggling to recover from repeated external shocks, necessitating root canal therapy.
# Darkened Tooth Color
As the pulp becomes infected, it can no longer provide vital nutrients. This causes the calcified tissues to darken and the tooth to appear grey or even black. Discoloration indicates pulp necrosis.
# Tissue Swelling
The pressure caused by an infected, inflamed pulp spreads to surrounding tissues. This manifests as puffy, inflamed gums around the affected tooth. Drainage and abscess formation can occur in severe cases.
# Recurring Gum Pimple
A persistent pimple-like bump on the gums near an infected tooth is called a fistula or sinus tract. This drainage pathway from the tooth root to the gum signals irreversible pulpitis and required root canal therapy.
# Large Prior Fillings
Teeth with extensive decay and restorative work are at higher risk for pulp infection due to recurrent decay or cracks that allow bacteria to infiltrate. Such teeth require diligent monitoring and often preemptive root canals.
# Trauma History
Injuries that result in pulp exposure immediately or later on frequently cause pulp necrosis. Whether from sports accidents, physical blows, or fractured teeth, trauma demands follow-up as root canals may be inevitable.
When multiple symptoms indicate sustained insult and inflammation, salvaging the tooth requires swift root canal intervention. Do not delay treatment, as the risks of pulp infections spreading quickly multiply. Seek professional care immediately.
III. What to do for tooth pain while waiting for a root canal?
Once root canal therapy is deemed necessary, you may have to wait days or even weeks for an appointment.
In the interim, severe tooth pain can disrupt sleep, work, and overall quality of life. While nothing but treatment will resolve the cause, several conservative measures can provide symptomatic relief:
# Over-the-Counter Pain Relievers
Non-prescription medicines like ibuprofen, naproxen or acetaminophen can help ease inflammation and dull nerve sensitivity. Use as directed.
# Cold Compresses
Applying an ice pack or cold washcloth to the exterior of the affected area constricts blood vessels, lowering pressure and inflammation. Use for 10-15 minutes at a time.
# Salt Water Rinses
Swishing and gargling with a warm salt water solution draws out fluid, reduces swelling, and keeps the area clean. Dissolve 1⁄2 teaspoon salt in 8 ounces of water.
# Dietary Adjustments
Avoid acidic, sugary, hot, or cold foods that could exacerbate nerve irritation and pain. Stick to lukewarm soft foods and hydrate with cool water.
# Sleeping Position
Keep your head elevated with pillows to allow drainage and reduce throbbing. Sleeping flat can worsen tooth pain.
# Topical Gels or Ointments
Products like Orajel contain benzocaine to numb contact points on the gums and provide temporary relief. Take care not to overuse it.
Though challenging, avoiding chewing on the affected side prevents further damage. Be sure to closely follow your dentist’s at-home recommendations while awaiting your procedure.
IV. What are the risks of avoiding a root canal when it’s needed?
When root canal therapy is recommended after a clinical examination, it is essential to schedule the appointment immediately rather than putting it off. Postponing necessary treatment allows the infection to progress and increase the risks of permanent complications:
# Spread of Infection
Without pulp removal, bacteria rapidly multiply within the tooth structure and infiltrate the root tips. This can lead to infections spreading through the jawbone or facial planes.
# Abscess Formation
Abscesses develop when infected pulp tissue dies and liquefies into pus that collects at the root tip. These pockets of pus won’t resolve without root canal disinfection.
# Risk of Tooth Loss
Without a blood supply, the tooth structure becomes brittle and vulnerable to fracture. Delaying treatment raises the chances of unavoidable extraction.
# Potential Systemic Effects
In rare cases, untreated oral infections can spread through the bloodstream and affect organs like the heart or brain. Prompt care is vital.
# Escalating Pain
As nerves die from sustained infection, pain may temporarily fade. But this calm precedes end-stage infection that returns with severe, frequent pain.
# Bone Loss
Expanding infection in the jawbone causes osteoclasts to increase bone resorption adjacent to the infected tooth. This can impact integrity.
Dental infections should never be ignored or postponed due to the risk of serious complications. Root canals stop disease progression in its tracks, avoiding the worst outcomes.
V. What If a Root Canal Is Not the Right Option for My Tooth?
While most diseased teeth can be salvaged with root canals, some may be too infected or structurally compromised to save. If non-restorable, the recommended options may include:
# Tooth Extraction
When an oral infection cannot be adequately treated or a tooth cannot be restored, removal of the tooth may be necessary. This completely eliminates the source of infection.
# Dental Implant
An artificial titanium screw implanted into the bone after extraction functionally replaces the missing tooth root. A crown is placed atop it for a natural appearance.
# Dental Bridge
This prosthetic appliance bridges the gap left by a missing tooth, adhering to adjacent teeth for support. It maintains structure and aesthetics.
# Removable Partial Denture
A removable acrylic device replaces multiple missing teeth with artificial replacements that can be taken out. It offers a budget-friendly solution.
# Pulp Capping
In cases of minor pulp exposure from trauma or decay, pulp capping can help heal and re-seal the pulp by placing a medicated dressing over the exposure site.
# Apicoectomy
When infection is isolated to the root tip, this surgical procedure removes just the root apex and seals the end. The majority of the tooth is left intact.
With modern techniques, many diseased teeth that once required extraction can now be salvaged through root canals or other conservative treatments. Discuss all options with your dentist.
VI. What are the best practices for oral hygiene to prevent cavities and root canals?
While heritage and anatomy play a role, there are many proactive steps you can take to maintain healthy teeth and gums:
# Brushing
Brush Thoroughly Twice Daily Use a soft-bristled brush and fluoride toothpaste to remove disease-causing plaque from tooth surfaces, paying special attention to where the teeth and gums meet. Take at least 2 minutes.
# Flossing
Floss at Least Once Daily Flossing removes plaque and food particles from between teeth that brushing misses. This helps prevent decay and periodontal disease.
# See Your Dentist Regularly
Professional cleanings and oral exams every 6 months spot issues early when they are easiest to treat. Your dentist can assess disease risk and recommend additional preventive measures.
Use Antimicrobial Rinses Swishing daily with antiseptic, antibacterial, or fluoride mouthwashes reduces oral bacteria between brushing and protects against cavities.
Watch Your Diet Limiting sugary foods and acidic drinks protects your enamel. Stay hydrated with water to help neutralize acids and rinse away carbohydrate residue.
Consider Fluoride Treatments Annual fluoride treatments create a reservoir effect, with fluoride incorporated into the enamel to make it more acid and decay-resistant. Discuss your risk factors with your dentist.
# Use Dental Sealants
These thin plastic coatings applied to the pits and grooves on the chewing surfaces of molars prevent food and plaque from getting trapped in these decay-prone areas.
# Wear Mouth Guards if Grinding
Clenching and grinding place enormous pressure on teeth, chipping enamel and exposing nerves. Custom night guards cushion this force.
With conscientious daily habits and regular professional care, your teeth can remain healthy and pain-free for decades to come.
VII. What foods should I avoid eating when I have a painful cavity?
When you have a cracked tooth, pulp inflammation, or a serious cavity causing discomfort, certain foods should be temporarily avoided to minimize pain levels and prevent further insult to the affected area:
- Sugary Foods – Hard candies, chocolates, sweet cereals, and sodas feed the plaque bacteria and worsen cavities and decay.
- Citrus Fruits – Acidic citrus fruits like oranges, lemons, and limes irritate exposed dentin and inflamed pulps.
- Carbonated Beverages – The bubbles and acidity in soda, beer, and sparkling water aggravate sensitive teeth.
- Ice Water or Ice Cream – Extreme cold shocks sensitive nerves in teeth with decay or cracks. Allow foods to warm closer to body temperature.
- Coffee and Tea – Hot beverages conduct heat directly to irritated pulp tissues and can exacerbate inflammation.
- Crunchy/Chewy Foods – Hard nuts, seeds, popcorn, bagels, taffy, granola bars, dried fruit, and the like put pressure on cracked or decayed areas.
- Alcoholic Beverages – Alcohol causes vasodilation that increases blood flow and fluid pressures on the dental pulp. Drink in moderation.
Sticking to a lukewarm, soft food diet gives symptomatic teeth a chance to settle down. Be sure to listen to the recommendations of your dentist.